We hope this update finds everyone well. It is springtime. Robin Williams once said “Spring is nature’s way of saying ‘Let’s party!’” Of springtime, Ernest Hemingway said, “When spring came, even the false spring, there were no problems except where to be the happiest.” It is with these happy seasonal thoughts we bring you this workers’ compensation update. The Texas legislative session continues and the Division of Workers’ Compensation recently held a Stakeholders meeting. The Division is also transitioning back to in-person contested case hearings. As always, if we can answer any questions or be of assistance, please contact us.
JOE AND BOB ARE SPEAKING AT THE INSURANCE COUNCIL OF TEXAS 4/21/2021 STATE OF THE TEXAS WORKERS’ COMPENSATION MARKET WEBINAR
Joe Anderson and Bob Graves are participating in a one-hour webinar, State of the Texas Workers’ Compensation Market, for the Insurance Council of Texas next Wednesday, April 21 at 11:00 a.m. This webinar has been approved by TDI for 1.0 hour of CE Credit – Course No.: 126290; and by the State Bar for 1.0 CLE Credits, Course No.: 174116874. It is going to be fun. If you are interested, please visit the ICT website.
LEGISLATIVE UPDATE
On January 12, 2021, the Legislature convened for the 87th Texas Legislative Session. Given the unprecedented impact of the COVID-19 pandemic, it will be an interesting Session to follow. The Legislature’s agenda reflects three top priorities: the budget, redistricting, and the pandemic. However, there have been some Legislative initiatives involving workers’ compensation. The following is a summary of some of the bills affecting workers’ compensation currently pending:
COVID Presumptions
A number of bills are pending that provide that certain employees are presumed to have contracted COVID-19 in the course and scope of employment. The types of employment addressed in these bills include:
- Public Safety Employees (First Responders/Detention Officers): HB 541, HB 637, HB 1498, HB 4301, SB 22, SB 107, SB 463, SB 527.
- First Responders: HB 34, HB 2073, SB 1401.
- School District Employees: SB 612.
- Nurses: HB 396, 433, 439.
These bills’ proposed presumptions may be rebutted. Most of the proposed presumption legislation provide that COVID-19 is not an ordinary disease of life regarding the employees covered by the presumption. Most of the bills provide for the application of presumption back to dates of injury after February, 2020. Some of the bills are specific to COVID-19, while others are tied to a disease for which the Governor makes a disaster declaration. Most of the debate regarding the bills concern parameters as to when the presumption starts and ends and “guard rails” to limit the presumption to only those intended to be covered.
Lifetime Income Benefits
The following pending bills address lifetime income benefits:
- HB 2502 — Addresses TBI, replaces incurable insanity or imbecility with mental illness or intellectual disability and adds LIBs entitlement for injury to spine that results in use of wheelchair for mobility. The bill also increases the benefit rate for first responders.
- HB 3120/SB 1450 — Addresses TBI, replaces incurable insanity or imbecility with permanent cognitive deficits that render employee unemployable and effect the non-vocational quality of life. The bill also adds LIBs entitlement for first responders who have an injury that results in permanent and total disability.
- HB 4038 — Addresses TBI, replaces incurable insanity or imbecility with mental illness or intellectual disability. The bill also adds LIBs entitlement for adhesive arachnoiditis. (an inflammatory disease that occurs inside the lumbar and sacral regions of the spinal canal).
PTSD
The following bills address PTSD and workers’ compensation:
- HB 3623 — Provides for the eligibility for workers’ compensation benefits for certain health care providers for PTSD arising from events in the course and scope of employment during public disaster.
- HB 2958 — Provides the date of injury for PTSD claim for first responders is the 30th day after the date the first responder is diagnosed with the disorder.
Medical Benefits
The following bills address medical benefits:
- HB 3098 — Permits DD and possibly RME exams regarding MMI/IR to be performed by telehealth/telemedicine services.
- HB 3818 — Requires payment of DD exam in event the claimant fails to appear. Also provides for increase in reimbursement of DD exams (tied to Consumer Price Index computed by Bureau of Labor Statistics).
- HB 4385 — Eliminates utilization review, giving deference to the treating doctor with Division oversight. Eliminates DD’s regarding MMI/IR determinations, giving presumptive weight to the treating doctor.
Regarding the Division
The following bills address obligations or duties by the Division of Workers’ Compensation:
- HB 1752 — Allows Division to conduct BRCs by videoconference or “in person, on showing of good cause.
- HB 1753 — Addresses time frames for certain required Division Reports.
- HB 1635 — Addresses research duties and reports of the workers’ compensation research and evaluation group.
- HB 2247 — Provides for a demonstration program at SORM for real-time processing of medical services/bills.
- HB 3042 — Permits the Division to, by rule amend or replace guidelines, protocols and formularies.
Approved Doctors
The following pending bills address the approved doctors for workers’ compensation:
- HB 3517/SB 1852 — Provides mechanism for reinstatement of treating doctor that was taken off the treating doctor list before 2007.
- HB 3622 — Prevents doctor removed from the treating doctor list before 2007 or who had their license suspended from treating workers’ compensation claimants, without exception, from treating workers’ compensation claimants.
Intoxication
HB 2654 addresses the definition of intoxication and replaces use of “glue or aerosol paint” with “volatile chemical” in definition of intoxication. The bill limits presumption of intoxication to “an analysis of specimen of blood, urine or any bodily fluid collected in an autopsy.” The bill provides the presumption of intoxication may be rebutted “only by credible and objective evidence that the person was not intoxicated.”
Death Benefits
HB 243 provides for a cost of living increase for death benefits tied to Consumer Price Index.
Mandatory Workers’ Compensation in Construction
HB 776 and SB 305 require contractors and subcontractors to provide workers’ compensation insurance coverage for each of their employees.
DIVISION’S STAKEHOLDERS QUARTERLY MEETING
The Texas Department of Insurance, Division of Workers’ Compensation Quarterly Stakeholders Meeting was held on April 9, 2021. Cassie Brown, Commissioner of the Texas Department of Insurance, Division of Workers’ Compensation made some brief opening remarks. She noted the Division was preparing for its Central Office move to the Austin Capitol Complex. This would result in some change of address concerns, which may affect some IT issues. She also briefly addressed the future transition back to in-person contested case hearings. Commissioner Brown explained that, since the COVID-19 pandemic, the Division had gone to virtual hearings. The Division was anxious to return to in-person contested case hearings. For the present, the Division will continue to conduct contested case hearings virtually. Commissioner Brown indicated the Division plans to return to in-person contested case hearings as soon as it believes such hearings would be safe. The Division is making some improvements to the contested case hearing rooms to provide for a safe hearing environment. The Division hopes to return to in-person hearings by summer 2021.
Commissioner Brown also highlighted the 2021 Workers’ Compensation Conference, titled “The Human Element,” which will be held virtually on June 28, 2021 through July 1, 2021. She indicated registration was currently open. Interested persons may learn more and register for the event at https://www.compevent.com/texas/.
Office of the Medical Advisor Update
Mary Landrum, Director of Health Care Business Management, provided an update for the Office of Medical Advisor (OMA). She explained that, for calendar year 2021, there had been 20 complaints forwarded to OMA. Fifty-five percent of these complaints were made by injured workers. Forty percent came internally from the Division and 5% were made by health care providers. A majority of the complaints concerned designated doctor exams. Other complaints concerned health care providers, peer reviews and required medical exam physicians. This year, OMA has investigated six complaints, with 83% closed with no action and 17% resulting in a medical quality review.
For this year, there have been nine medical quality reviews initiated. One review was concluded and referred to Enforcement.
For this year, two cases were closed by Enforcement, one with a consent order and one with a warning letter. Twenty-two OMA cases remain pending in Enforcement and two OMA cases remain pending at the State Office of Administrative Hearings (SOAH). Director Landrum also touched on health care providers who have been removed from the workers’ compensation system. She reminded system participants that the consent orders removing health care providers from the system could be found on the Division’s website.
Compliance and Investigations Update
Debra Knight, Deputy Commission of Compliance and Investigations, provided an update regarding compliance and investigations. She explained that, so far, in 2021, the Division has received 317 complaints. The complaints fell into the following categories:
- Attendance (3);
- Communications (91);
- Fraud (0);
- Indemnity benefit delivery (90);
- Medical benefit delivery (68);
- Other (50); and
- Quality of Care (12).
Three hundred and nine of the complaints have been closed. Of those, in 106 the Division confirmed a violation occurred. In 48 of the complaints, an education letter was issued. Of the 309 closed complaints, the Division was unable to confirm a violation occurred in 155.
Deputy Commissioner Knight addressed the Division’s ongoing compliance audits. The Division is currently conducting death benefits and lifetime income benefits audits. Nineteen have been completed and four are in progress. Deputy Commission Knight noted a trend regarding these audits, indicating the Division continues to identify instances where benefits were being paid at the incorrect rate. This is typically a result of benefits being paid without an accurate wage statement or, in the case of lifetime income benefits, failure to account for the 3% annual increase.
Deputy Commissioner Knight briefly touched upon 2020’s Performance Based Oversight (PBO) assessments. In 2020, the Division assessed 120 insurance carriers. Forty were found to be high performers. Seventy-six were found to be average performers and four were found to be poor performers. Deputy Commissioner Knight noted that 22 of the carriers reviewed in 2020 were not previously reviewed in the last assessment. Deputy Commissioner Knight also indicated they were in the process of developing a PBO assessment process for the 2021 PBO assessment of health care providers.
Regarding fraud, Deputy Commissioner Knight noted that in 2021 there have been 223 fraud referrals received by the Division. One hundred and eleven fraud cases were opened. Fifty-six fraud cases were closed and there were two fraud referrals for prosecution. There have been five indictments for fraud in 2021, all involving attorneys. This year, there have been 12 fraud convictions, all concerning health care providers.
Deputy Commissioner Knight touched upon the Division’s enforcement actions. She provided examples of typical administrative violations by the insurance carriers, which include:
- Failure to timely pay indemnity benefits;
- Failure to timely initiate TIBs;
- Failure to accurately pay TIBs;
- Failure to investigate a claim;
- Attorney fee violations; and
- Failure to comply with a Division decision or order.
Currently, there are 361 pending enforcement cases. Of those, 92 involve health care providers, 257 involve insurance carriers and 12 involve other parties. Of the enforcement cases closed, the Division has issued warning letters to 26 health care providers and 17 carriers. The Division issued orders in 10 cases involving a health care provider and 15 cases involving carriers.
Designated Doctor Update
Joe McElrath, Deputy Commissioner of Business Process, gave a brief update regarding designated doctors. He noted that, as of June 20, 2020, the Division reinstated the designated doctor process following its suspension because of COVID-19. Since the reinstatement of the designated doctor process, designated doctors have not been permitted to address disability or return to work issues. Deputy Commissioner McElrath acknowledged that, in November of 2020, the Texas Workforce Commission reinstated its requirements that individuals make work search efforts in order to obtain unemployment benefits. However, he noted that the Division’s similar requirement regarding work search efforts by claimants to receive supplemental income benefits (SIBs) remains suspended. He indicated the Division would provide sufficient notice to all system participants before reinstating the work search requirements associated with SIBs.
Deputy Commissioner McElrath explained that designated doctors, currently, may not address issues related to disability and return to work. The Division has been holding parties’ requests for designated doctors to address these issues and will process those requests when the Division lifts the restrictions on designated doctor exams. He indicated that some of the requests had been pending for some time and the Division will reach out to the parties to determine whether the designated doctor exam is still needed, before scheduling the exam.
Deputy Commissioner McElrath explained the Division was continuing to revise the Prospective Employment Authorization and Certification form (Form 156). The revised form should be completed in the near future. Deputy Commissioner McElrath also reminded system participants the revised Request for Records Check or Copy of Confidential Claim Information (Form 153) has been adopted and is being used by system participants. The revised form does not required notarized signatures, may be electronically submitted and records may be received electronically.
Deputy Commissioner McElrath also addressed the Division’s Central Office move to the Capital Complex next year. He indicated the Division will have a change in its post office box address. Likewise, due to the move and address changes, there will be some modification to Division forms. Deputy Commissioner McElrath indicated the Division would reach out to system participants regarding changes associated with communications and forms.
Updates on Electronic Data Interchange (EDI)
Martha Luévano, Director of Enterprise Automation Services (EAS), provided an update on EDI. She initially address the EDI technical work group. She explained they recently met on April 7, 2021 and primarily discussed the transition to EDI R3.1. They are continuing to take steps the implementation of EDI R3.1 and will continue to hold meetings in the summer. If a system participant wishes to join the technical work group, Director Luévano encouraged them to email the Division at edisupport@tdi.texas.gov.
Director Luévano went over EDI reporting of initial TIBs and medical bills. System participant reporting of this information remains consistent with past years.
Director Luévano also touched upon the ability of carriers to make changes to the claim record via EDI. She noted that the carrier may make an EDI change through a report 148-02 or FROI 02 when a change is necessary regarding the injured employee’s address/phone number or employer information. A carrier may make a change in the same way regarding an update of a jurisdictional SSN 999-MM/DDYY to a real SSN. However, this change would have to be reviewed by staff before it would be allowed to pass through.
Changes regarding social security number, date of injury, employee’s first/last name or an employee’s birthdate need to be emailed to records/processing@tdi.texas.gov.
Director Luévano also addressed coding issues related to adverse reactions to the COVID-19 vaccine. She indicated system participants are to use to Code 38 when addressing adverse reactions to a vaccine. She specifically instructed participants not to use Code 83, which is limited to COVID-19.
Director Luévano indicated system participants continue to receive error code 058/ID invalid. She requested system participants continue to report these instances to edisupport@tdi.texas.gov. She further encouraged system participants who were having issues with rejections, connectivity, or to self-report a violation, to contact the Division at edisupport@tdi.texas.gov.
Legislative Update
Jeff Nelson, Director of External Relations, gave a legislative update. He briefly covered the following current pending legislation.
Hearings Update
Kerry Sullivan, Deputy Commissioner of Hearings, gave a hearings update. He briefly explained that, while there has been an increase in proceedings where continuances were granted, more proceedings are occurring as scheduled. He further noted that the number of agreements reached at Benefit Review Conferences (BRCs) remains consistent with previous years
Deputy Commissioner Sullivan indicated there are some scheduling changes occurring in hearings. Hearings may be reassigned to a different presiding officer than originally scheduled. This may occur the week before the scheduled proceeding. Notice for these changes will be sent by email and the subject of the email should say “Urgent-Updated Zoom Information.” The new Zoom information will be contained in the email.
Deputy Commissioner Sullivan also addressed electronic documents used at the CCHs. He indicated that, due to the virtual nature of hearings, it is important that the number of pages indicated on the cover sheet of any document submitted be consistent with the actual number of pages in the document. Likewise, exhibits should be properly labeled and numbered consecutively, if possible. He noted documents and exhibits are allowed to be electronically submitted at CCHs via secured file transfer protocol (SFTP). He indicated this process may be used to upload both exhibits as well as videos. He encouraged participants to use the proper naming conventions, which are provided when you sign up for an SFTP account. If you want to set up an SFTP account, Deputy Commissioner Sullivan instructed participants to contact DWC at efiling-help@tdi.texas.gov. Deputy Commissioner Sullivan also encouraged all system participants please use video in virtual proceedings. Appearing by video instead of simply by audio, provides for a smoother functioning proceeding.
COVID-19 Data Call Update
Amy Lee, Special Advisor/Director Research and Evaluation Group, addressed the COVID-19 data call and update. She explained the Division has been monitoring COVID-19 claims reported to an insurer as of February 14, 2021. There have been approximately 44,873 claims identified, including 200 fatalities. In an effort to research and evaluate these claims, the Division has been conducting data calls. The Division categorized COVID-19 claims by occupation (using industry codes), which reflected:
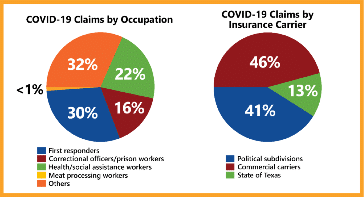
The Division also categorized the claim by industry, showing the following:
- 48% public administration.
- 22% healthcare and social assistance.
- 6% administrative and support in waste management and remediation services.
- 4% educational services.
- 4% manufacturing.
- 4% retail trade.
- 3% accommodation and food services.
- 2% transportation and warehousing.
- 7% all other industries.
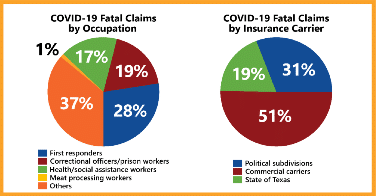
Regarding fatal COVID-19 claims, the Division’s data reflected:
The data call showed the following as of December 31, 2020:
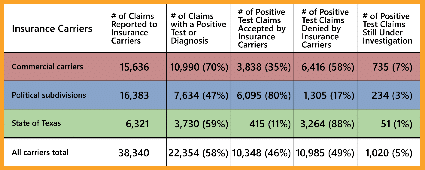
Regarding workers’ compensation benefits associated with COVID-19, $21.2 million in indemnity benefits have been paid. Fifty percent of that consists of income benefits and 47% is associated with employers’ salary continuation. There have been $12.4 million in medical benefits paid. Eighty percent of the medical benefits paid is for hospital/facility services.
MFDR Update
Greg Arendt, Director of Medical Fee Dispute, provided an update regarding medical fee disputes. His update focused primarily on the recent changes to Division Rule 133.307, which became effective on February 22, 2021. The changes allow health care providers to submit a medical fee dispute by “secure file transfer protocol, fax, encrypted email, any mail service or personal delivery.” The changes also provide that an insurance carrier response to a medical fee dispute will be deemed timely “if received by the Division through mail services, personal delivery or electronic transmission, as described in §102.5 of this title within 14 days after the date that respondent received a copy of the requestor’s dispute.” Regarding whether a dispute is considered timely submitted, before the rule was amended, a dispute was considered received on the date the MFDR section received the request for medical dispute resolution. The rule now provides that the dispute is considered received on the date the Division receives the request.
Director Arendt also addressed the Division’s new search tool regarding MFDR decisions. It can be located at the Division’s website.
Following Director Arendt’s presentation, Commissioner Brown gave some closing remarks and the quarterly meeting was then concluded.
DIVISION TRANSITIONING TO IN-PERSON CONTESTED CASE HEARINGS AUGUST 2, 2021
The Division of Workers’ Compensation has been monitoring the latest developments related to COVID-19. Due to increasing vaccine availability and ongoing safety improvements to field offices, the Division has determined that in-person contested case hearings will resume Monday, August 2, 2021. The Division encourages all system participants to begin preparing for these in-person contested case hearings. In the coming weeks, dockets will begin to reflect this future change. Parties should continue to electronically file and exchange documents.